Aortic stenosis is one of the most common and clinically significant heart valve diseases worldwide. It affects millions of people, particularly older adults, and can have serious consequences if left untreated. The condition involves a narrowing of the aortic valve opening, which restricts blood flow from the left ventricle to the aorta and the rest of the body. Over time, this increased workload on the heart can lead to heart failure, arrhythmias, and even sudden cardiac death.
This article provides a comprehensive, medically accurate, and easy-to-understand overview of aortic stenosis, including its causes, symptoms, diagnostic methods, progression, and modern treatment options.
Understanding the Aortic Valve and Its Function
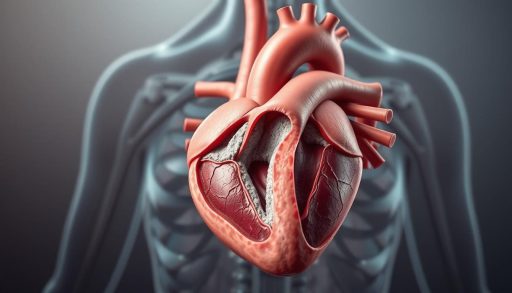
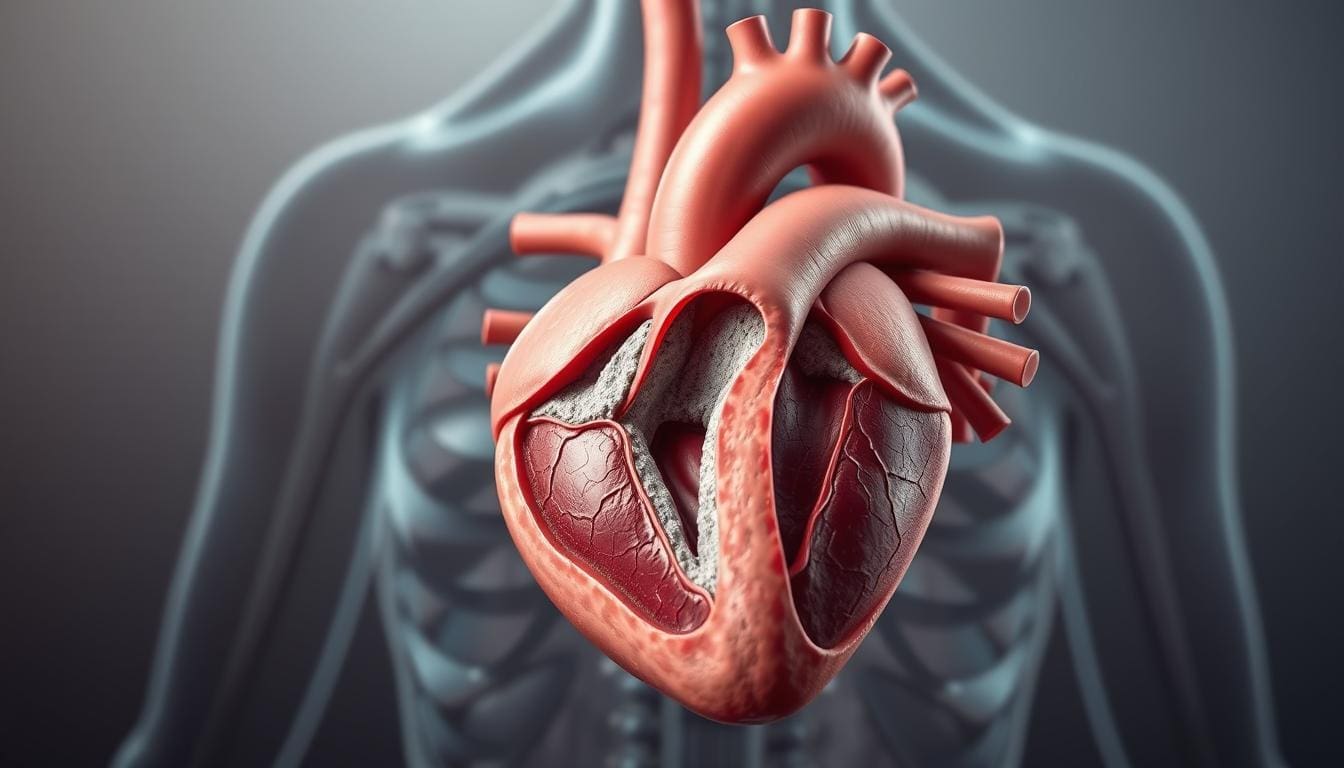
The heart has four valves: the mitral, tricuspid, pulmonary, and aortic valves. The aortic valve plays a critical role in maintaining efficient blood circulation. It opens to allow oxygen-rich blood to flow from the left ventricle into the aorta and then closes to prevent backflow.
A healthy aortic valve opens fully with each heartbeat, allowing blood to move freely. In aortic stenosis, the valve becomes narrowed, stiff, or thickened, reducing its ability to open properly. This obstruction forces the heart to work harder to pump blood, leading to structural and functional changes in the heart muscle.
What Is Aortic Stenosis?
Aortic stenosis is a progressive condition characterized by the narrowing of the aortic valve opening. As the valve area decreases, blood flow becomes increasingly restricted. The left ventricle must generate higher pressure to overcome this resistance, which can eventually cause ventricular hypertrophy (thickening of the heart muscle) and impaired cardiac function.
The severity of aortic stenosis is typically classified as:
-
Mild
-
Moderate
-
Severe
-
Critical
In its early stages, the condition may remain asymptomatic for years. However, once symptoms appear, the prognosis worsens significantly without proper treatment.
Causes of Aortic Stenosis
Several factors can contribute to the development of aortic stenosis. The most common causes include:
1. Age-Related Calcification
In older adults, calcium deposits can build up on the aortic valve over time. This calcification causes the valve leaflets to stiffen and narrow, reducing their ability to open fully. This is the leading cause of aortic stenosis in people over the age of 65.
2. Congenital Heart Defects
Some individuals are born with abnormal aortic valves, such as a bicuspid valve (two leaflets instead of three). These valves are more prone to early degeneration and calcification, often leading to aortic stenosis at a younger age.
3. Rheumatic Heart Disease
Although less common in developed countries, rheumatic fever can damage the aortic valve. The resulting scarring and fusion of valve leaflets can cause narrowing and impaired function.
4. Radiation Therapy
Radiation to the chest area, especially during cancer treatment, can increase the risk of valve disease years later.
Risk Factors
Several factors increase the likelihood of developing aortic stenosis:
-
Advanced age
-
High blood pressure
-
High cholesterol
-
Smoking
-
Diabetes
-
Chronic kidney disease
-
Family history of valve disease
Lifestyle and metabolic factors play a significant role in accelerating valve calcification.
Symptoms of Aortic Stenosis
Aortic stenosis often develops slowly, and symptoms may not appear until the condition becomes severe. When symptoms do occur, they typically include:
1. Chest Pain (Angina)
Reduced blood flow can limit oxygen delivery to the heart muscle, causing chest discomfort, especially during physical exertion.
2. Shortness of Breath
As the heart struggles to pump efficiently, fluid can accumulate in the lungs, leading to breathlessness, particularly during activity or when lying down.
3. Fatigue
Decreased blood flow to the body can result in persistent tiredness and reduced exercise tolerance.
4. Dizziness or Fainting
Insufficient blood flow to the brain may cause lightheadedness or syncope, especially during physical exertion.
5. Heart Palpitations
Some patients experience irregular heartbeats due to changes in heart structure and electrical conduction.
6. Swelling in the Legs or Feet
In advanced stages, heart failure can cause fluid retention in the lower extremities.
How Aortic Stenosis Progresses
The progression of aortic stenosis varies from person to person. Some individuals remain stable for many years, while others experience rapid worsening.
Once symptoms appear, the average survival rate without intervention decreases significantly:
-
Angina: ~5 years
-
Syncope: ~3 years
-
Heart failure: ~2 years
This highlights the importance of early diagnosis and timely treatment.
Diagnosis of Aortic Stenosis
Accurate diagnosis relies on a combination of clinical evaluation and imaging studies.
1. Physical Examination
A heart murmur, caused by turbulent blood flow through the narrowed valve, is often the first clue. The murmur is typically heard with a stethoscope during routine exams.
2. Echocardiography
This is the gold standard for diagnosing aortic stenosis. Ultrasound imaging provides detailed information about:
-
Valve structure
-
Valve area
-
Blood flow velocity
-
Pressure gradients
-
Left ventricular function
3. Electrocardiogram (ECG)
An ECG can reveal signs of left ventricular hypertrophy or rhythm abnormalities.
4. Chest X-ray
This may show heart enlargement or calcium deposits on the valve.
5. Cardiac CT or MRI
Advanced imaging can assess valve anatomy and calcium burden with high precision.
6. Cardiac Catheterization
In selected cases, invasive testing is used to measure pressure differences across the valve.
Severity Classification
Aortic stenosis is classified based on valve area and pressure gradients:
| Severity | Valve Area | Mean Gradient |
|---|---|---|
| Mild | >1.5 cm² | <20 mmHg |
| Moderate | 1.0–1.5 cm² | 20–40 mmHg |
| Severe | <1.0 cm² | >40 mmHg |
This classification helps guide treatment decisions.
Treatment Options for Aortic Stenosis
There is no medication that can reverse aortic stenosis. Treatment focuses on managing symptoms and replacing the diseased valve when necessary.
1. Medical Management
In mild cases, doctors may recommend:
-
Blood pressure control
-
Cholesterol management
-
Diuretics for fluid retention
-
Regular monitoring
However, medications cannot fix the narrowed valve.
2. Surgical Aortic Valve Replacement (SAVR)
Traditional open-heart surgery involves removing the damaged valve and replacing it with a mechanical or biological prosthesis.
Advantages:
-
Long-term durability
-
Excellent outcomes in suitable patients
Disadvantages:
-
Requires open surgery
-
Longer recovery time
3. Transcatheter Aortic Valve Replacement (TAVR)
TAVR is a minimally invasive procedure in which a new valve is inserted through a catheter, usually via the femoral artery.
Benefits:
-
Shorter recovery
-
Less invasive
-
Suitable for high-risk patients
TAVR has become a standard option for many patients, including those with moderate surgical risk.
4. Balloon Aortic Valvuloplasty
This procedure temporarily widens the valve opening using a balloon catheter. It is typically used as a bridge to definitive treatment.
Types of Replacement Valves
Mechanical Valves
-
Very durable
-
Require lifelong blood thinners
-
Higher bleeding risk
Biological (Tissue) Valves
-
Made from animal tissue
-
No long-term anticoagulation
-
Limited lifespan (10–20 years)
The choice depends on age, lifestyle, and medical conditions.
Recovery and Long-Term Outlook
After valve replacement, most patients experience significant symptom improvement and better quality of life. Regular follow-up is essential to monitor valve function and overall heart health.
Lifestyle recommendations include:
-
Heart-healthy diet
-
Regular physical activity
-
Smoking cessation
-
Blood pressure control
With proper treatment, many patients live full, active lives.
Complications of Untreated Aortic Stenosis
If left untreated, severe aortic stenosis can lead to:
-
Heart failure
-
Arrhythmias
-
Stroke
-
Sudden cardiac death
-
Reduced life expectancy
Early intervention dramatically improves survival rates.
Aortic Stenosis in Younger Patients
Although more common in older adults, aortic stenosis can affect younger individuals with congenital valve abnormalities. These patients often require lifelong monitoring and may need multiple interventions over time.
Advances in Research and Future Therapies
Ongoing research focuses on:
-
Improved valve materials
-
Longer-lasting biological valves
-
Less invasive procedures
-
Early detection methods
Artificial intelligence and advanced imaging are also enhancing diagnostic accuracy.
Living With Aortic Stenosis
Patients diagnosed with aortic stenosis can maintain a good quality of life by:
-
Attending regular check-ups
-
Reporting new symptoms promptly
-
Following medical advice
-
Staying physically active within limits
Education and awareness are key to managing the condition effectively.
When to See a Doctor
You should seek medical evaluation if you experience:
-
Persistent chest pain
-
Shortness of breath
-
Dizziness or fainting
-
Unexplained fatigue
Early diagnosis can be life-saving.
Aortic stenosis is a serious but treatable heart condition. Advances in medical technology have transformed patient outcomes, offering safer and more effective treatment options than ever before. With proper diagnosis, timely intervention, and ongoing care, individuals with aortic stenosis can enjoy a longer, healthier, and more active life.
Understanding the disease, recognizing symptoms early, and working closely with healthcare professionals are essential steps toward optimal heart health.